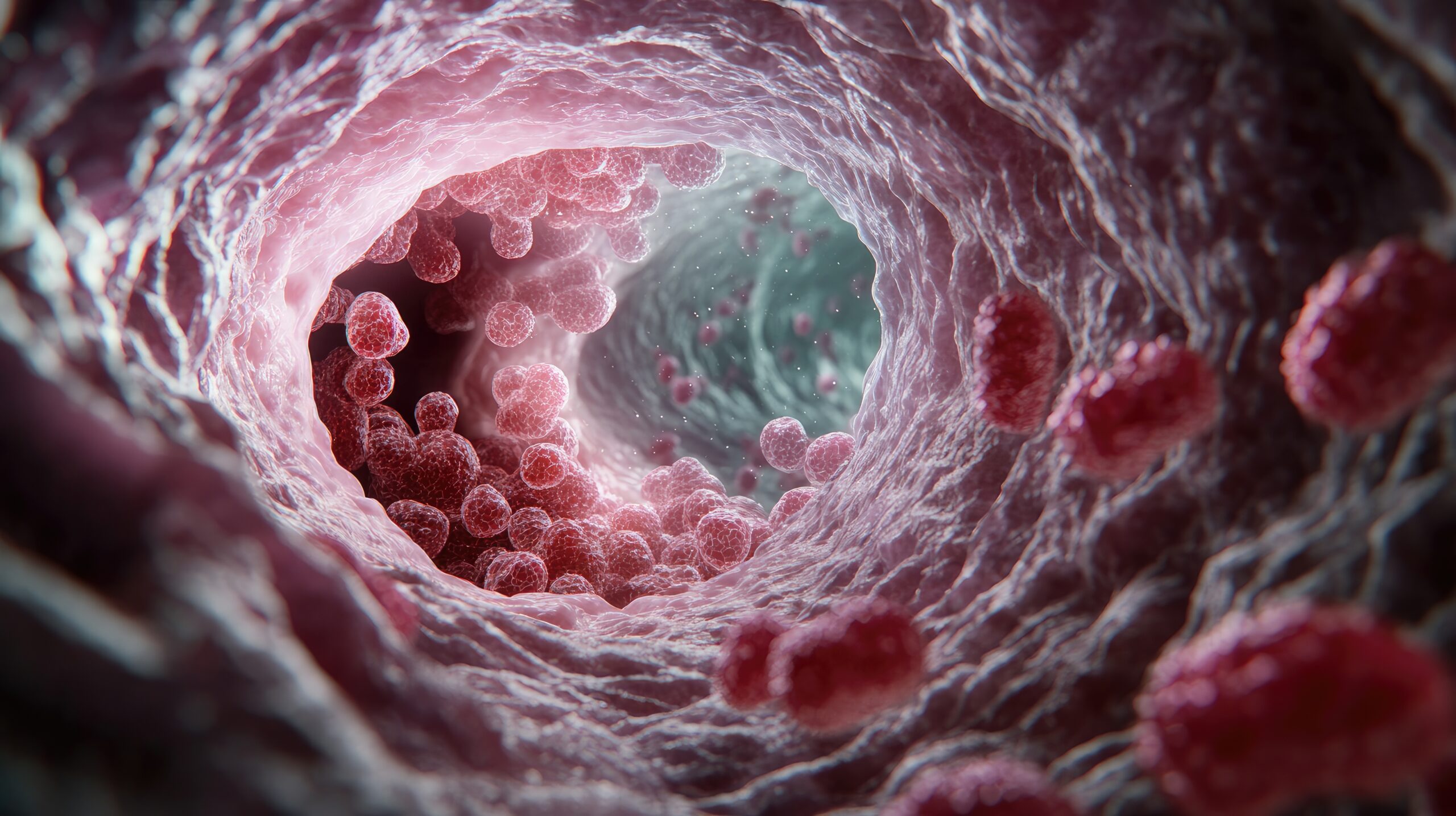
Eosinophilic oesophagitis (EoE) is a chronic, immune-mediated inflammatory disease of the oesophagus that is progressive in nature and increasingly prevalent worldwide.1 The condition is driven by antigen-induced type 2 inflammation, leading to the infiltration of eosinophils, which causes esophageal dysfunction and related symptoms. For some with EoE, current treatments are insufficient to control the condition, creating a need for new therapeutic options.2 Results from a recent phase 3 clinical trial (NCT04753697), presented at UEG Week 2024, has shown promising results for cendakimab (CEN), a monoclonal antibody targeting interleukin (IL)-13, a cytokine thought to be a key driver of inflammation in EoE.1,3
The trial was a multicenter, multinational, randomized, double-blind, placebo (PBO)-controlled study designed to investigate CEN’s effectiveness in reducing oesophageal inflammation and improving symptoms in both adult and adolescent patients. Participants ranged from 12 to 75 years of age, all had active EoE that had not fully responded to ≥ 8 weeks of proton pump inhibitor treatment, and all had experienced at least 4 days of dysphagia within the 14 days prior to the trial.
A total of 430 patients were enrolled and randomized in a 1:1:1 ratio to receive one of three treatment regimens: subcutaneous CEN 360 mg weekly for 48 weeks (n = 143, QW/QW), CEN 360 mg weekly for 24 weeks followed by 360 mg every other week for the next 24 weeks (n = 143, QW/Q2W), or PBO weekly (n = 144) for 48 weeks. Approximately 66% of the participants were steroid inadequate responders or intolerant. The trial’s coprimary endpoints were mean change in dysphagia days from baseline to week 24 to assess symptom improvement, and the proportion of individuals with an eosinophil histologic response, defined as a peak eosinophil count (PEC) of ≤ 6 eosinophils per high-power field (hpf) at week 24. Safety was also evaluated, along with a series of secondary endpoints, including the proportion of patients with eosinophil histologic response (< 15 eos/hpf) at week 24, endoscopic response (measured by changes in Endoscopic Reference Score [EREFS]), EoE Histology Scoring System (EoEHSS) grade and stage, and changes in the modified Daily Symptom Diary (mDSD) composite score from baseline to week 24.
Key findings from the study demonstrated that in patients treated with CEN 360 mg QW (n = 286), there was a statistically significant reduction from baseline to week 24 in dysphagia days vs PBO (−6.1 vs −4.2 days; difference [95% CI] vs PBO:−1.9 [−3.0 to −0.8]; P=0.0005) and a statistically significantly higher proportion of patients with an eosinophil histologic response at week 24 vs PBO (28.6% vs 2.2%; difference [95% CI] vs PBO: 26.4 [20.6 to 32.2]; P< 0.0001).
Beyond these primary outcomes, CEN 360 mg QW also showed statistically significant improvements across all secondary endpoints measured. In terms of safety and tolerability, by week 24, adverse events (AEs) related to the drug were reported in 30.3% of patients in patients receiving CEN 360 mg QW and 18.9% in the PBO group. AEs led to discontinuation in 1.4% of CEN-treated patients and 0.7% of those on PBO, and no deaths were reported.
In summary, the trial investigators concluded that treatment with CEN resulted in statistically significant improvements in both symptoms and the histologic and endoscopic features of EoE compared to PBO, and that CEN was generally safe and well-tolerated up to week 24.
References
1. Barchi A, Mandarino FV, Yacoub M-R, Albarello L, Massimino L, Savarino EV, Ungaro F, Passaretti S, Masclee GMC, Danese S, et al. From Pathogenesis to Treatment: Targeting Type-2 Inflammation in Eosinophilic Esophagitis. Biomolecules. 2024; 14(9):1080. doi.org/10.3390/biom14091080
2. Lucendo AJ, López-Sánchez P. Targeted Therapies for Eosinophilic Gastrointestinal Disorders. BioDrugs. 2020 Aug;34(4):477-493. doi: 10.1007/s40259-020-00427-w.
3. Schoephfer AM, et al. Cendakimab efficacy and safety in adult and adolescent patients with eosinophilic esophagitis: 24-week results from the randomized, placebo-controlled, phase 3 study. Abstract LB11. UEG Week 2024.
Disclosure: This article was created by the touchIMMUNOLOGY team utilizing AI as an editorial tool (ChatGPT (GPT-4o) [Large language model]. https://chat.openai.com/chat.) The content was developed and edited by human editors. No funding was received in the publication of this article.