Search Results
Showing Results for inflammatory

Metabolic dysfunction-associated steatohepatitis (MASH) is a progressive liver disease driven by fat build-up and immune activation, often linked to obesity and diabetes. Emerging therapies target both metabolic and immune pathways, showing promise in reducing inflammation, improving liver function, and reversing fibrosis. These advances offer hope for better management of this complex disease.

The American College of Gastroenterology’s 2025 Crohn’s disease guidelines introduce key advancements in personalized care, diagnostics, and treatment. Highlights include genetic testing to guide therapy, adoption of intestinal ultrasound for non-invasive monitoring, and the inclusion of new biologics. Emphasizing shared decision-making and holistic care, the guidelines aim to improve outcomes by tailoring strategies to each patient’s unique profile and preferences.

As part of our EULAR 2025 coverage, Dr Dinesh Khanna discusses early findings from the Breakfree-1 trial investigating BMS-986353, a next-generation CD19 CAR T-cell therapy, in severe, treatment-refractory autoimmune diseases. In this exclusive interview, Dr Khanna explores the rationale, mechanism, and encouraging early results in systemic sclerosis, highlighting robust CAR T expansion, immune reset, and meaningful clinical improvements in skin and lung outcomes.
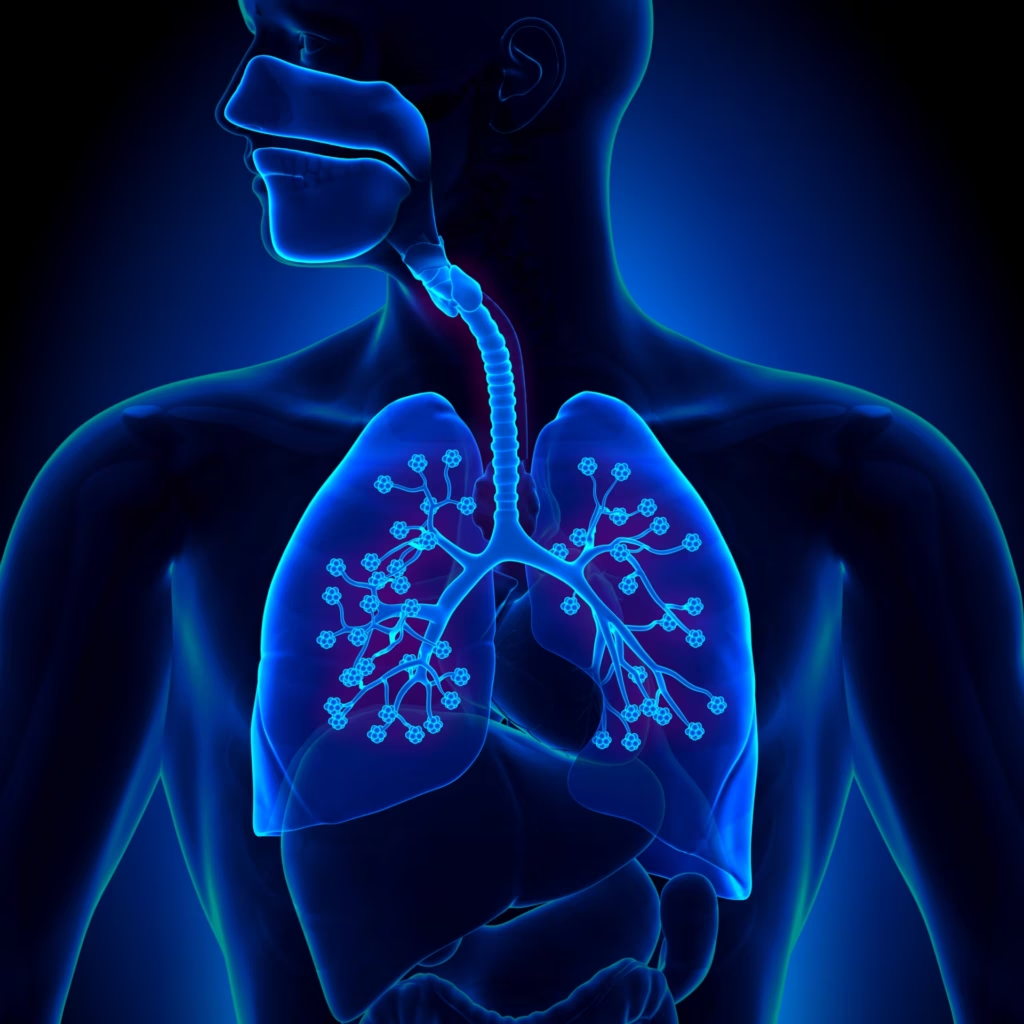
Interstitial lung disease (ILD) is a common and potentially fatal complication of systemic autoimmune rheumatic diseases (SARDs), such as rheumatoid arthritis (RA) and systemic sclerosis (SSc). ILD may be the first sign of disease or develop later, often with variable clinical courses. Early detection is critical, as delayed diagnosis contributes to poor outcomes. In response, the 2023 American College of Rheumatology (ACR) guidelines emphasize routine screening and risk-based strategies to improve identification and management of SARD-associated ILD (SARD-ILD).

In this Future Leaders interview, Dr Salvatore Oliva discusses his path to paediatric gastroenterology, highlighting his focus on chronic inflammatory conditions like IBD and EGIDs. He shares insights on leading European collaborative research, the integration of innovation into clinical care, and the promise of precision medicine. Dr Oliva also offers guidance for early-career doctors drawn to this dynamic and multidisciplinary field.

Physician burnout is at a critical point. In this episode, Nicky speaks with Dr Alfred Atanda about why so many physicians are burning out and what can be done to change the trend. From personal experience to system-wide solutions, Dr Atanda shares valuable insights on improving physician well-being and building a more effective healthcare culture.

As part of our Future Leaders series, we spotlight Dr Sonali Bracken, a physician-scientist at Duke University advancing rheumatologic care through cutting-edge research on B cells in autoimmunity. Recently awarded the 2024 ACR Distinguished Fellow Award, Dr Bracken shares insights into her path, research focus, and the emerging therapies poised to transform patient outcomes.

As part of our coverage of DDW 2025, we speak with Dr Florian Rieder about the STENOVA trial evaluating AGMB-129 in fibrostenosing Crohn’s disease. He discusses the rationale behind targeting the TGF-β pathway, the trial design, and promising interim findings suggesting localized efficacy and improved stricture symptoms without systemic toxicity.
In this episode, we explore the future of continuing medical education (CME) with the team behind touchIME. Hannah Fisher and Matthew Goodwin share insights into global and US trends, the importance of patient inclusivity and how educational outcomes are evolving to better measure the direct impact of learning on clinical practice and patient care.

Dr. Vinod Ravindran (Centre for Rheumatology, Calicut, Kerala, India) shares his highlights from RheumaPreg 2025, held in Vienna. The conference covered the full spectrum of pregnancy management in autoimmune rheumatic diseases. Here, he reflects on key insights from expert-led sessions on fertility, immunosuppression, lupus care, and postpartum outcomes.

Nominated Future Leader, Dr Tom Appleton, shares insights into his career, osteoarthritis research, and the role of immunology in shaping future OA treatments. In this interview, Dr Appleton discusses the importance of early intervention, the impact of synovial macrophage dysfunction, and emerging therapies that could revolutionize rheumatology. His work bridges clinical care and research to drive innovation in osteoarthritis management and autoimmune disease.

In the interview, Dr Paul Pockros discusses his presentation from DDW 2025 on the SPRING study (NCT04595825), which evaluated CM-101, a novel anti-CCL24 monoclonal antibody, in adults with primary sclerosing cholangitis (PSC). With no FDA-approved treatments for PSC, CM-101 showed promising safety, tolerability, and biomarker improvements over 48 weeks, supporting advancement to phase 3 trials.

At the 2025 WCO-IOF-ESCEO congress, Professor Philip Conaghan presented the safety and efficacy findings from the phase 2 study of LEVI-04 for the treatment of adults with knee osteoarthritis. LEVI-04 is a first-in-class, NT-3 inhibitor, which works by targeting the inflammatory pathways involved in joint degeneration and selectively inhibiting pro-inflammatory cytokines.

The European Commission has approved upadacitinib for treating giant cell arteritis (GCA) in adults. This marks the first oral JAK inhibitor approved for GCA in the EU. Backed by the findings from the phase III SELECT-GCA trial, upadacitinib offers a new option for managing this chronic inflammatory disease in adults.
With a career that spans continents, Prof. Dedee Murrell stands out as a global leader in dermatology and a passionate advocate for women in medicine. In this episode, we sit down together to explore her inspiring journey—from her early years in the UK and medical training in the USA to pioneering therapies for some of dermatology’s rarest and underserved conditions in Australia. We also reflect on her recent MDS Lifetime Achievement Award and discuss the value of mentorship, strategies for advancing a career in dermatology and academic medicine, and how to stay at the cutting edge of medical innovation.

New research has shown that infliximab clearance is increased in patients hospitalized with severe ulcerative colitis, potentially leading to a higher risk of underexposure when standard dosing regimens are used. The study, which analyzed infliximab pharmacokinetics in 154 patients with ulcerative colitis, found that patients who were hospitalized exhibited a 35% increase in infliximab clearance compared to outpatients (0.463 L/day vs. 0.339 L/day, p<0.0001). This resulted in subtherapeutic drug levels in the majority of patients from week 2 onwards, with 74% of hospitalized patients having infliximab concentrations below 20 µg/mL at week 2, 69% below 15 µg/mL at week 6, and 56% below 7 µg/mL at week 14.
Latest articles videos and clinical updates - straight to your inbox
Log into your Touch Account
Earn and track your CME credits on the go, save articles for later, and follow the latest congress coverage.
Register now for FREE Access
Register for free to hear about the latest expert-led education, peer-reviewed articles, conference highlights, and innovative CME activities.
Sign up with an Email
Or use a Social Account.
This Functionality is for
Members Only
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.



