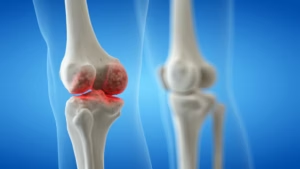
 Osteoarthritis (OA) is the most common form of arthritis and a leading cause of pain and disability, particularly in older adults.1 Current treatment options are largely symptomatic, relying on pain relief through NSAIDs, corticosteroid injections, and, in severe cases, joint replacement surgery. These approaches do not modify the disease course and are associated with side effects, especially with long-term use. No disease-modifying osteoarthritis drugs (DMOADs) have been approved for routine clinical use, highlighting a major unmet need.2
Osteoarthritis (OA) is the most common form of arthritis and a leading cause of pain and disability, particularly in older adults.1 Current treatment options are largely symptomatic, relying on pain relief through NSAIDs, corticosteroid injections, and, in severe cases, joint replacement surgery. These approaches do not modify the disease course and are associated with side effects, especially with long-term use. No disease-modifying osteoarthritis drugs (DMOADs) have been approved for routine clinical use, highlighting a major unmet need.2
Evidence now shows that OA is not a single disease but a collection of heterogeneous conditions with diverse clinical phenotypes and molecular endotypes.3 This complexity has contributed to the failure of many DMOADs in late-phase trials. As such, there is increasing momentum towards personalised medicine in OA, which aims to classify patients into more precise subtypes to guide targeted therapies.4
In this Q&A, Dr Ali Mobasheri (Professor of Musculoskeletal Biology, University of Oulu, Oulu, Finland) discusses the challenges of defining patient subgroups in clinical practice, the role of patient stratification in accelerating therapy development, and the long-term potential of personalised approaches to improve outcomes and reduce the overall burden of OA.
The abstract ‘Advancing osteoarthritis trials and therapeutic development through clinical phenotyping and molecular endotyping’ was presented at WCO-IOF-ESCEO, 10–13 April, 2025.
Q. What are the main challenges in defining OA phenotypes and endotypes clinically?
OA is no longer considered a homogeneous disease characterised by “wear and tear”. Instead, it is being viewed as a highly heterogeneous disease, with diverse clinical phenotypes and underlying biological mechanisms. One major challenge lies in the absence of standardised criteria to clearly delineate clinical phenotypes and molecular endotypes in a clinical setting. Clinical phenotypes are based on observable phenotypic traits like pain severity, joint location, and radiographic changes, which often overlap and evolve over time. Molecular endotypes are biologically distinct subgroups defined by molecular pathways. They are the pathogenic drivers of the disease but they are even more difficult to identify without access to advanced ‘omics’ platforms and biomarker assays, which are never integrated into routine clinical practice. They are primarily used in research and clinical trials. Furthermore, the lack of large, deeply phenotyped and well-characterised patient cohorts with matched clinical, imaging, and molecular data hampers efforts to validate proposed subtypes and apply them meaningfully in clinical trials or routine healthcare practice.
Q. How might clinical phenotyping and molecular endotyping accelerate personalised therapy development in OA?
By understanding OA, not as a single disease but as a spectrum of distinct subtypes, we can begin to develop and tailor therapies to the right patients. Clinical phenotyping helps identify patients with shared disease features, while molecular endotyping uncovers the underlying mechanisms, such as inflammation, cartilage degeneration, or subchondral bone remodelling, that drive disease in each subgroup. This approach enhances clinical trial design for patients that are most likely to respond to specific and targeted interventions, thus increasing the likelihood of demonstrating efficacy of a pharmaceutical or biological agent. Over time, this precision medicine focused strategy could guide real-world therapeutic decisions, allowing clinicians to select treatments based on a patient’s clinical phenotype and the underlying biological drivers of their disease.
Q. How can patient subtyping help the development of targeted DMOADs?
Many DMOADs have failed in late-phase trials, in part due to the “one-size-fits-all” approach to patient recruitment. Patient subtyping allows us to select individuals whose disease is driven by mechanisms directly targeted by that intervention. These could be driven by inflammation, cartilage degradation, or bone remodelling. This increases the signal-to-noise ratio in trials, improving our ability to detect meaningful treatment effects. Subtyping also opens the door to drug repurposing and combination therapies tailored to specific endotypes, potentially transforming the way we think about OA drug development and hopefully reducing clinical trial failures and attrition in the clinical development pipeline.
Q. What are the most promising molecular markers for OA subtyping?
At this point in time, there are no single biomarkers that can be used for subtyping. The idea is to use a combination of biomarkers. We are doing some work in this area to identify panels of biomarkers that can be used to characterise the different types. Watch this space for updates from our group and collaborators!
Q. How could this personalised approach to OA treatment impact patients in the long term?
A personalised approach promises to revolutionise the way OA care is delivered. By matching the right treatment to the right patient at the right time, we can improve clinical outcomes, preserve the joint and delay arthroplasty. In fact, the regulatory agencies want to see drugs impacting pain, function and joint survival. The regulators prioritise impacts on pain and function and recognise the need for reducing surgical interventions like joint replacement. Using a personalised approach may also reduce the trial-and-error prescribing of symptomatic treatments, reducing the adverse side-effects of painkillers, improving quality of life for the patient and reducing healthcare costs. Ultimately, this personalised strategy could shift OA management from “reactive” to “proactive”, enabling earlier intervention and disease modification based on a patient’s individual risk profile and a molecular or even genetic signature.
References:
- Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. The Lancet. 2019;393:1745–59.
- Guermazi A, Roemer FW, Crema MD, et al. Strategic application of imaging in DMOAD clinical trials: focus on eligibility, drug delivery, and semiquantitative assessment of structural progression. Ther Adv Musculoskelet Dis. 2023;15. Doi: 10.1177/1759720X231165558
- Mobasheri A, van Spil WE, Budd E, et al. Osteoarthritis Year in Review 2021: Molecular Pathology and Personalized Medicine. Osteoarthritis and Cartilage. 2021;29:1249–60.
- Mobasheri A, Loeser R. Clinical phenotypes, molecular endotypes and theratypes in OA therapeutic development. Nat Rev Rheumatol. 2024;20:525–6.
Further content in osteoarthritis.
Editor: Victoria Jones, Senior Content Editor.
Disclosures: This short article was prepared by touchIMMUNOLOGY in collaboration with Ali Mobasheri. touchIMMUNOLOGY utilize AI as an editorial tool (ChatGPT (GPT-4o) [Large language model]. https://chat.openai.com/chat.) The content was developed and edited by human editors. No fees or funding were associated with its publication.
Ali Mobasheri discloses consulting for and participating in speaker’s bureaus with: Sanofi, Opella, Viatris, HALEON, Aptissen, Contura, Laboratoires Expanscience, ACI, Sunac Therapeutics, Ampio Pharmaceuticals, Synartro, Bruder Consulting and Venture Group, Chiron, Chondropeptix, Grünenthal, Hypera Pharma, ICM, Kangstem, Kolon Life Science, Kolon TissueGene, SynOA Therapeutics, Nestlé Health Science, Pluri, Enlivex, Apos Health, and Pacira Biosciences; receiving grant/research support from: Research Council of Lithuania / Lietuvos mokslo taryba, Research Council of Finland / Suomen Akatemia and the European Commission; serving on advisory boards for: ESCEO; receiving honoraria from: various international societies; and being a major stock/shareholder in: Sunac Therapeutics.
Cite: Clinical Phenotyping and Molecular Endotyping in Osteoarthritis – Personalised Approaches to Therapeutics: Ali Mobasheri, WCO-IOF-ESCEO 2025. touchIMMUNOLOGY. April 2025.
SIGN UP to TouchIMMUNOLOGY!
Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out.