Rheumatoid arthritis (RA) is one of the most challenging autoimmune diseases. Early, targeted and effective therapy is crucial for achieving remission and preventing long-term joint destruction. Over the past two decades, tumour necrosis factor (TNF) inhibitors (TNFi) have been the mainstay of first-line biotherapy, delivering transformative outcomes for many patients. However, despite their efficacy, their current administration remains suboptimal. Fixed dosing strategies are broadly applied, ignoring patient-specific factors such as body weight, smoking status and baseline inflammatory burden. These factors can profoundly influence treatment response. Interestingly, while TNFi therapy appears to be sensitive to body mass index (BMI), other biologics, such as tocilizumab and abatacept, seem to be less affected by obesity, suggesting that drug-specific pharmacokinetics should be considered when optimizing treatment.1 We need to exploit the ‘window of opportunity’ that exists in the early stages of RA – a critical period to achieve sustained disease control. By failing to personalize TNFi therapy, we risk suboptimal treatment responses, premature switching to other therapies and a subsequent reduction in the probability of achieving remission.
The ‘window of opportunity’ and the need for personalization
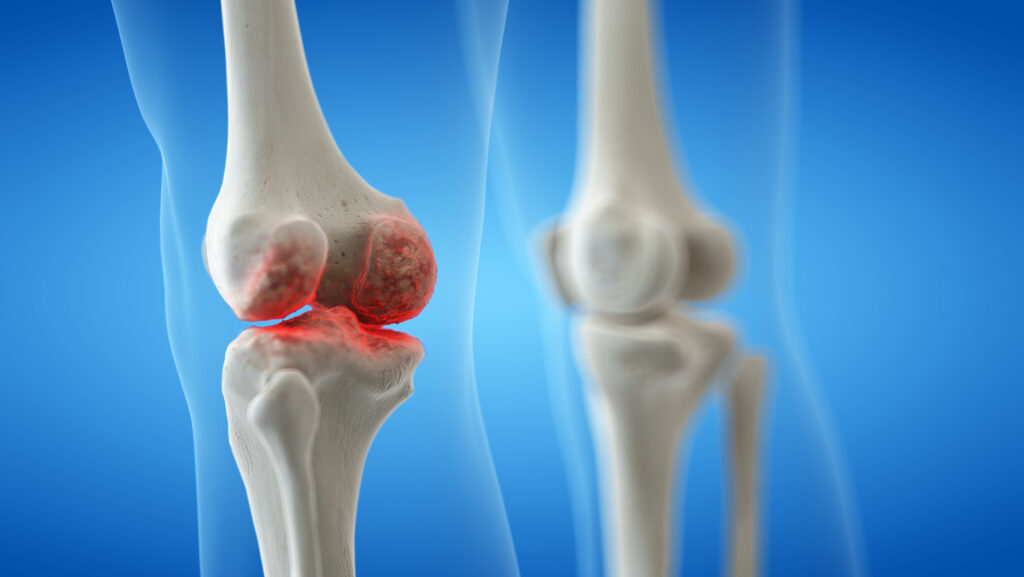
The ‘window of opportunity’ in RA refers to an early phase of the disease during which prompt intervention can significantly alter its course. Early treatment during this period has been shown to improve long-term outcomes, including the prevention of joint damage and sustained remission.2,3 This concept has been extensively validated in RA, emphasizing the need for early and optimized therapeutic intervention.
TNFi are effective in managing RA, but their efficacy can be influenced by individual patient factors. For instance, obesity is associated with reduced response to TNFi therapy, possibly due to altered drug pharmacokinetics.4 Smoking is another factor that can negatively impact TNFi treatment outcomes. Studies have shown that current smoking is associated with worse functional status in patients with RA, suggesting a diminished response to therapy.5 Additionally, the high-titre rheumatoid factor has been implicated in differential responses to TNFi agents, influencing treatment efficacy and possibly guiding therapeutic selection.6 It is also crucial for patients with a high baseline inflammatory burden to have their dose adjusted or treatment strategy intensified to achieve optimal disease control. Despite the evidence supporting the influence of these factors on treatment response, standardized dosing regimens are often applied without considering individual patient characteristics, potentially leading to suboptimal outcomes.7 Thus, integrating these patient-specific elements into treatment decision-making could enhance the effectiveness of TNFi therapy in RA.
Lessons from gastroenterology: Individualized approaches
The lack of optimization in RA management contrasts sharply with advancements made in other inflammatory diseases, such as inflammatory bowel disease (IBD). In gastroenterology, personalized approaches to TNFi therapy have demonstrated significant benefits. For instance, proactive therapeutic drug monitoring is routinely employed to optimize dosing. Evidence from studies, such as those on subcutaneous infliximab (CT-P13 SC) as a maintenance therapy for patients with IBD, highlights the feasibility and efficacy of individualized treatment approaches.8 Similarly, the REMSWITCH study (A 24-month real-life persistence, efficacy and safety study in IBD patients in remission switched from intravenous infliximab to subcutaneous infliximab CT-P13; ClinicalTrials.gov identifier: NCT04990258) demonstrated the effectiveness and safety of transitioning patients from intravenous to subcutaneous infliximab, ensuring sustained drug efficacy while adapting to patient needs.9 Furthermore, a recent single-cell sequencing study provided crucial insights into the molecular effects of anti-TNF therapies in IBD, highlighting an approach that could be applied to RA research to refine personalized treatment strategies.10
One argument against optimizing TNFi therapy in RA has been the supposed variability and noise in disease activity measures such as the Disease Activity Score 28. However, when compared with IBD, Crohn Disease Activity Index scores are similarly complex, increasing confidence in the comparison of IBD to RA in terms of the possibility of distinguishing when to alter the dose.
Emerging evidence in rheumatology
Emerging research in rheumatology is beginning to mirror the personalized approaches seen in gastroenterology. Recent studies have demonstrated the value of therapeutic drug monitoring in TNFi therapy for RA and psoriatic arthritis, showing that drug levels and the presence of anti-drug antibodies (ADA) closely correlate with treatment outcomes.11 Factors such as BMI, adherence to therapy and concurrent use of disease-modifying antirheumatic drugs were identified as significant determinants of TNFi efficacy. However, a recent meta-analysis highlighted that no single molecular biomarker, including anti-citrullinated protein antibodies, consistently predicts anti-TNF efficacy, suggesting that composite or artificial intelligence (AI)-driven biomarker combinations may be needed to achieve truly predictive precision medicine in RA.12
Measuring trough levels has been proposed as a practical approach to guide clinical decisions, including dosage adjustments, therapy intensification or switching within the TNFi class or to a biologic with an alternative mechanism of action.13,14 In particular, a recent study demonstrated that monitoring TNFi trough levels and detecting ADA can significantly improve disease management.15 Additionally, innovative tools, such as machine-learning models based on multi-omics data, show promise in predicting individual patient responses to TNFi therapy.16 By integrating data on genetic, transcriptomic and proteomic markers, these models provide a framework for precision medicine in rheumatology. A molecular classifier biomarker test has also been developed to enrich for non-response to TNFi, providing a valuable tool in guiding therapeutic choices.17 Such approaches could enable rheumatologists to optimize TNFi therapy proactively, improving remission rates and reducing adverse effects.
Implications of non-optimization
This lack of optimization has serious implications for patient outcomes. Inadequate disease control in the first-line setting leads to premature switching to alternative therapies, which may not yield the same results. Data show that patients who fail TNFi therapy are less likely to respond robustly to subsequent biological treatments, limiting their options and jeopardizing long-term disease control. Failure to optimize first-line TNFi therapy represents a missed opportunity to align RA management with the principles of precision medicine, which emphasize tailoring treatment strategies to individual patient profiles.13
Strategies for optimization
We must rethink and optimize the use of TNFi agents as first-line therapy in RA. There are several strategies to address this challenge.
-
Tailoring dosages based on patient-specific factors, such as body weight or inflammatory burden, ensures adequate drug exposure and improves response rates. While the inflammatory burden is intuitively a strong predictor, current biomarker analyses have not yet identified a single predictive factor, suggesting that a more nuanced or composite approach may be required.18
-
Biomarker-driven approaches with early identification of poor responders through predictive biomarkers, including drug levels and anti-drug antibody status, allow for timely dose escalation or treatment modifications. Although current meta-analyses have not identified definitive predictive biomarkers, AI-driven biomarker combinations may improve treatment stratification in the future.
-
Proactive monitoring through frequent assessments of clinical response and disease activity enables early intervention, preventing irreversible damage.
Conclusion
A more personalized approach to TNFi therapy is key to enhancing outcomes in RA. By ensuring that patients receive the right dose of the right drug at the right time, we can maximize the benefits of TNFi agents, improve the likelihood of achieving remission and reduce the risk of premature treatment failure. While precision medicine in RA remains an evolving field, current strategies to refine treatment approaches represent a critical step forward.