Standardization of the assessment of disease activity in patients with rheumatoid arthritis (RA) has made a big difference in the comparability of clinical trials and in treatment processes in clinical practice.1–3 Disease activity is the underlying driver for radiographic progression, and functional limitations and functional disabilities may also evolve by progressive structural damage.4,5 The introduction of composite disease activity indices like the Disease Activity Score in the 1990s and the Simplified/Clinical Disease Activity Index (SDAI/CDAI) in the 2000s have incorporated the different perspectives of disease activity in a single outcome.6
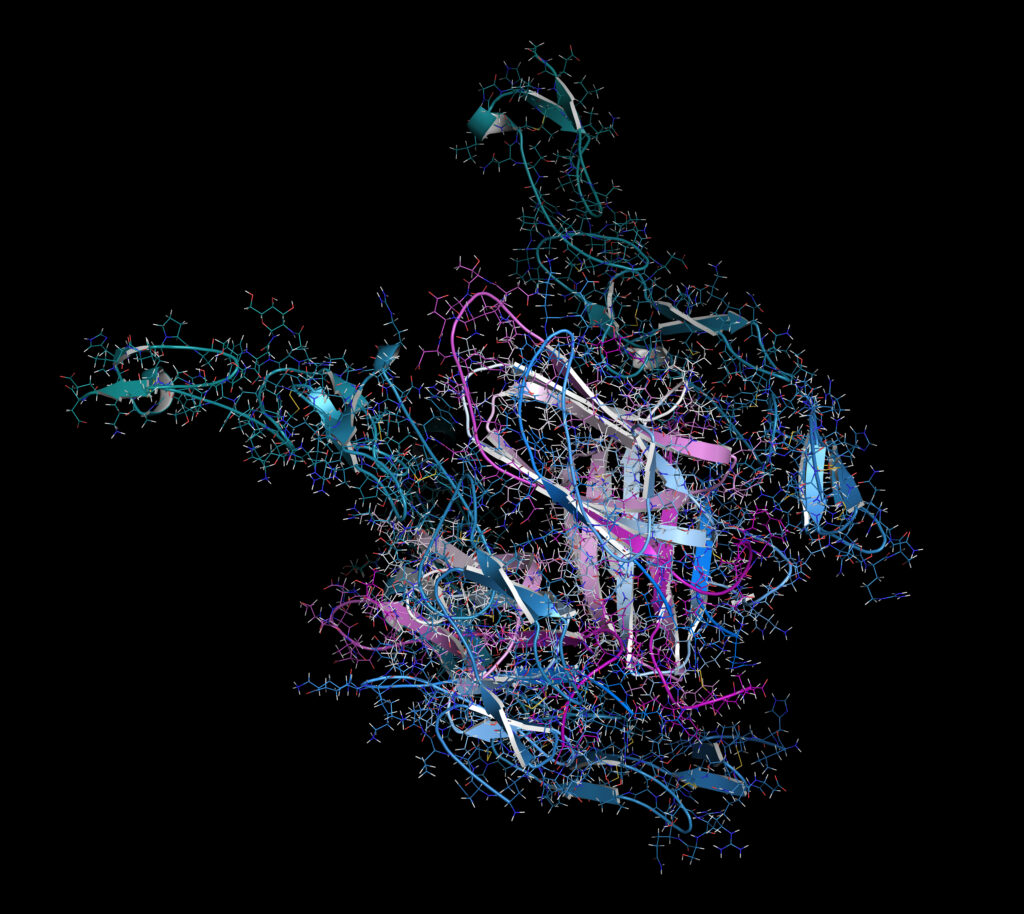
Over the past three decades, our treatment armamentarium has increased immensely, with several pathways involved in inflammation targeted by disease-modifying antirheumatic drugs. The treat-to-target strategy, initially introduced in 2010,7 has now been implemented in many rheumatology clinics and has proven to lead to better outcomes for our patients.8 The ultimate goal in the management of patients with RA is to achieve a state of remission or, if this is not attainable, low disease activity. This process needs to be accompanied by shared decision making, ideally in partnership with patients. Remission is defined as the absence or near absence of inflammation and should coincide with stable long-term outcomes, including no (further) radiographic progression as well as only marginal, if at all, functional limitations.
The 2011 American College of Rheumatology/European Alliance of Associations for Rheumatology (ACR/EULAR) remission criteria for RA outline the guidance for classifying patients in remission.9 These criteria were based on the interpretation and consensus by a large internal consortium analysing several trial data sets. The main results were the definition of remission using a Boolean approach and a SDAI or CDAI cut-off of 3.3 or 2.8, respectively. The Boolean definition in its final version incorporated the Swollen Joint Count 28 (SJC28), Tender Joint Count 28 (TJC28), Patient Global Assessment (PtGA) and C-reactive protein (in mg/dl). To classify a patient in remission, none of these parameters should be above 1. In particular, the combination of SJC28 and TJC28 with an additional more subjective measure of disease activity was analysed in detail. The PtGA coincided with higher likelihood ratios for predictive validity on combined good functional and radiographic long-term outcomes than pain or the evaluator global assessment.9
Since its publication in 2011, the ACR/EULAR remission criteria have been discussed in several reports, including if they are stringent enough thus allowing for residual disease activity, or too stringent with the risk of potential overtreatment.10,11 In particular, the PtGA has been the subject of debate since it was the criterion most often not fulfilled, despite fulfillment of the other three criteria, and ultimately the most common limiting factor for reaching clinical remission, followed by SJC28.12,13 It has been demonstrated, that while SJC28 is the major determinant of physician global assessment, PtGA is mainly driven by pain.14 Findings that the level of agreement between patient-reported joint pain and tenderness is similar as the level of tenderness and swelling on a joint adds another piece to the puzzle of relationships between these outcomes.15 Taken together, it may be suggested that pain, tenderness and swelling are, to some extent, different concepts with heterogenous implications.
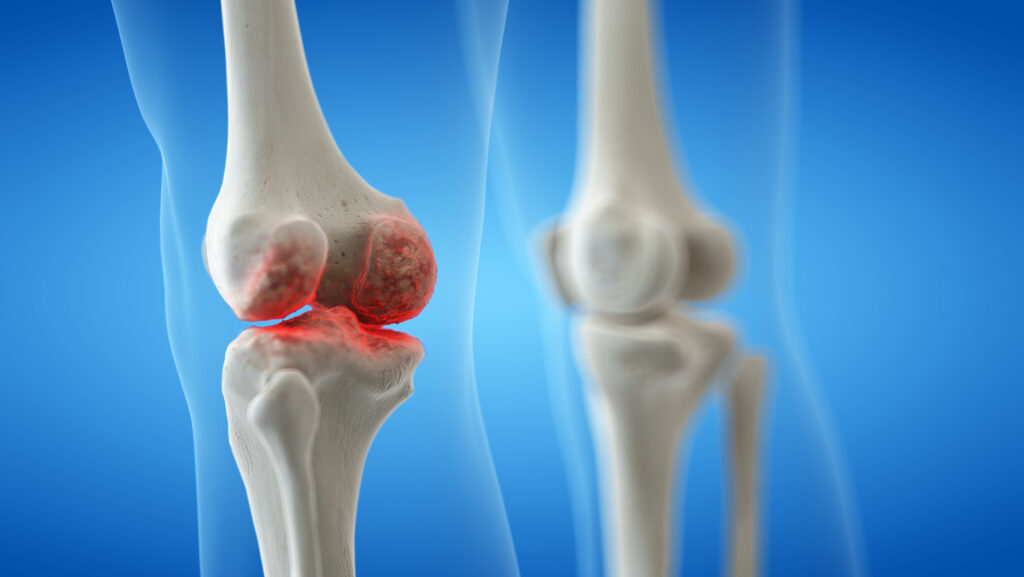
A systematic literature review of randomized controlled trials and longitudinal cohort studies highlighted that in regard to single components, only objective markers of inflammation (i.e. SJC and C-reactive protein) may act as predictors of radiographic progression, as opposed to semi-objective (TJC) or subjective (pain, PtGA) markers.16 As swollen joints are stronger predictors of radiographic progression than systemic inflammatory markers,17 aiming for the lowest possible number of swollen joints is the best strategy to prevent damage and retain functionality.18 A recent observational study, however, also noted that in some cases, tender non-swollen joints may undergo structural damage.19
The ARCTIC trial investigated the value of the treat-to-target strategy using imaging as an additional outcome, but the study has not found a superiority in terms of long-term outcomes.20 It could also underpin the relationship of the index-based and the Boolean remission definition with combined functional and radiographic long-term outcomes.21
Nearly 10 years after the publication of the ACR/EULAR remission criteria, the influence of increasing the threshold of the PtGA within the Boolean criteria on face, convergent and predictive validity was investigated.22 Using six clinical trial datasets, including 2,600 early and established patients with RA, it was shown that a somewhat higher threshold for the PtGA increases the agreement with index-based criteria, but does not interfere with the predictive validity of the criteria.23–28 An omission of the PtGA, however, would lead to a reduced homogeneity in identifying the same patients independent of the definition used and is associated with worse functional, but not radiographic, outcomes. A PtGA threshold of 2 out of 10 or 20 on a visual analogue scale from 0 to 100 mm coincided with higher agreement with the SDAI remission definition, independent of the statistical method used.
The ACR/EULAR remission criteria were provisionally endorsed in 2011, but have since not been officially validated in independent datasets. Furthermore, the proposed revision of Boolean criteria needed external validation to receive endorsement. A further study that included patient data from four randomized controlled trials, which originally investigated disease-modifying antirheumatic drugs directed against interleukin 6, CD20 and tumour necrosis factor, analysed the validity of revising the Boolean criteria (Boolean 2.0) and the provisionally endorsed index-based criteria.29,30 In patients with early RA, 92% instead of 71% (94% instead of 74% in established RA) could achieve the Boolean criteria along with SDAI remission, when using a PtGA threshold of 2 cm compared to 1 cm. In established RA, the agreement decreased when a threshold above 2 cm for the PtGA was used. The Boolean 2.0 criteria were now fulfilled by 20% of patients with early RA and 6% of patients with established RA, similar to the frequencies for SDAI and CDAI remission (19% in early RA and 5% in established RA) after 6 months of treatment. Since the PtGA has been criticized as the criterion that most patients struggle to fulfill for being classified in Boolean remission, by using Boolean 2.0 the rate of ‘near misses’ due to PtGA has reduced from 61% to 47%. In terms of predictive validity, particularly for combined long-term outcomes, Boolean 2.0 showed similar performance as Boolean 1.0 and the index-based definitions. The report of these results has been reviewed by the ACR and EULAR committees and received full endorsement in 2022.
For the evaluation of remission in people with RA, any of the outlined 2022 criteria may be used since all show similar validity in early and established RA. However, patient assessment in clinical practice should be put in context with regard to the individuals’ sociocultural health, since any assessment can be skewed by the influence of factors such as comorbidities. Above all standardization processes, the management and clinical decision making should be based on a shared decision between rheumatologists and patients. It is expected that the revised remission criteria will be tested in observational studies to highlight aspects in real-world scenarios.